Squint – How I Do It
Paediatric Ophthamology & Strabismus
Abstract
Introduction: Squint is a condition where there is misalignment of the visual axes[1]. Common types include esotropia and exotropia while hypertropias are not very common[1]. This article seeks to describe how I carry out squint surgeries secondary to either head injuries, cerebral palsies (CP), cerebral visual impairment, cataract or any other cause in my practice.
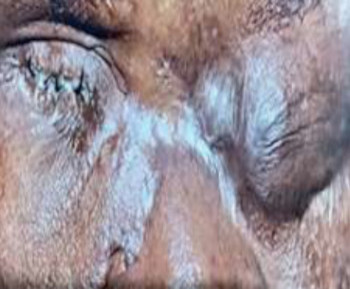
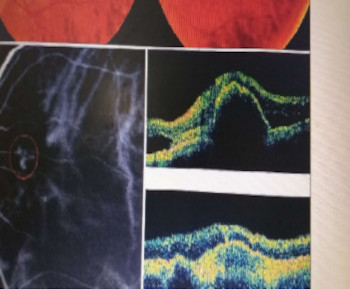
Methods: My first steps involve carrying out general examination of the child’s overall appearance, level of alertness during history taking, noting any head posture, and gross ocular alignment. I also generally assess a child with dysmorphic features. I always examine the systems such as the cardiovascular, abdominal, chest, musculoskeletal and central nervous systems. For ocular examination, I usually assess visual acuity using preverbal and verbal techniques as appropriate. I then observe fixation for monofixation or binocularity. In monocular fixation I test for central, steady and maintained fixation or fix and follow gaze. Eccentric fixation is an important sign as this shows that the patient is not fixing with the fovea and vision is in the range of 20/200 or worse. I examine the child or adult appropriately looking for media opacities, refraction, other tests, stereopsis, etc. I refer children to paediatricians for systemic evaluation and invite anaesthetists to examine the child to confirm fitness for surgery. Pre- operatively, I nsist the patients use prophylactic topical antibiotics and maintain good personal and facial hygiene. After proper examination and preparation for surgery, children are usually done under general anaesthesia while adults are done under local anaesthesia
References
von Noorden GK, Campos EC. Binocular Vision and Ocular Motility. In: Theory and Management of Strabismus. 6th ed. St. Louis: Mosby, 2001; 246-247.
Chuka-Okosa MC. Amblyopia: Types, presentation and treatment- A review. Niger J Ophthalmol 2003; 11:54-62.
Carlton J, Karnon J, Czoski-Murray C, Smith KJ, Marr J. The clinical effective and cost-effectiveness of screening programs for amblyopia and trabismus in children up to the age of 4–5 years; a systemic review and economic evaluation. Health Technol Assess 2008; 12:1–194.
Akpe AB. Strabismus and Amblyopia amongst Primary School Pupil in Egor Local Government Area, Benin City. Fellowship Dissertation. National Postgraduate Medical College of Nigeria, Lagos, 2010; 16-25.
Megbelayin EO. Prevalence of Amblyopia amongst Secondary School Students in Calabar, South-South, Nigeria. Niger J Med 2012; 21:407- 411.
Ajaiyeoba AI, Isawumi MA, Adeoye AI, Oluleye TS. Prevalence and Causes of Eye Diseases amongst Students in SouthWestern Nigeria. nnals of African Medicine 2006; 5:197-203.
Ayanniyi AA, Mahmoud AO, Olatunji FO. Causes and prevalence of ocular morbidity among primary school children in Ilorin, Nigeria. Niger J Clin Pract 2010; 13:248-253.
Nkanga DO, Dolin P. School vision screening programme in Enugu, Nigeria: Assessment of referral criteria for errors of refraction. Niger J Ophthalmol 1997; 5:30-40.
Adegbehingbe BO, Oladehinde MK, Majengbasan TO, Onakpoya HO, Osagiede EO. Screening of Adolescents for Eye Diseases in Nigerian High Schools. Ghana Med J 2005; 39: 138-142.
Onyekwe LO, Ajaiyeoba AI, Malu KN. Visual impairment amongst school children and adolescent in Jos, Nigeria. Niger J Ophthalmol 1998; 6:1-5.
Robaei D, Rose K, Ojaimi E et al. Causes and Associations of Amblyopia in a Population-Based Sample of 6-Year-Old Australian Children. rch Ophthalmol 2006; 124:878-884.
Mohammad M, Masoud A, Hamid M, Ramak R. Associations of refractive amblyopia in a population of Iranian children. J Optom 2012; 12:1- 6.
Mohamed D, Yiong-Huak C, Gus G et al. Prevalence of Refractive Error in Singaporean Chinese Children: The Strabismus, Amblyopia, and Refractive Error in Young Singaporean Children Study (STARS). Invest Ophthalmol Vis Sci 2010;51:1348-1355.
Pai AS, Rose KA, Leone JF et al. Amblyopia Prevalence and Risk Factors in Australian Preschool Children: The Sydney Paediatric Eye Disease Study (SPEDS). Ophthalmology 2012; 119:138- 144.
The Joint Writing Committee for the Multiethnic Paediatric Eye Disease Study and the Baltimore Paediatric Eye Disease Study Groups. Risk Factors for Decreased Visual Acuity in Preschool Children: The Multi-Ethnic Pediatric Eye Disease and Baltimore Pediatric Eye Disease Studies. Ophthalmology 2011; 118:2262-2273.
The Joint Writing Committee for the Multiethnic Paediatric Eye Disease Study and the Baltimore Paediatric Eye Disease Study Groups. Risk Factors Associated with Childhood Strabismus: The MultiEthnic Pediatric Eye Disease and Baltimore Pediatric Eye Disease Studies. Ophthalmology 2011; 118:225-2261.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Transactions of the Ophthalmological Society of Nigeria

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.