Ocular Loiasis: Still Existent in this Millennium - A Case Report
Abstract
Background: Loiasis is a neglected tropical, vector-borne parasitic disease due to a nematode Loa loa and transmitted to humans by deerfly, genus Chrysops. [1,2,3] Loiasis is endemic in the tropical rainforest belts of Central and West Africa including Nigeria. [1,2,3,4]
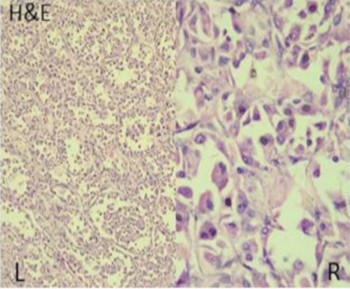
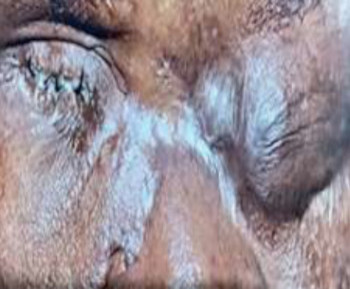
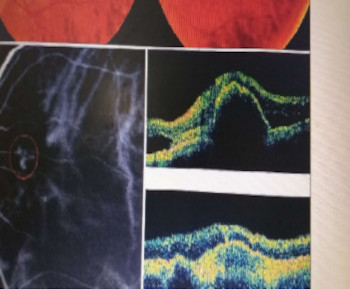
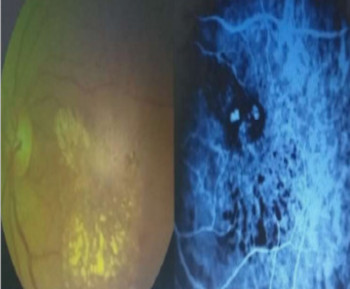
The emergence of loiasis as a disease of public health importance, is not only because of its endemicity but also of its impediment on the control of onchocerciasis and lymphatic filariasis in areas of co-endemicity. [1,5] The clinical manifestations of loiasis characteristically include: localized angioedema ound predominantly on the extremities (Calabar swelling), pruritus, and Subconjunctival migration of the adult L. loa worm. The subconjunctival and/ or palpebral migration of the adult L. loa worm and angioedema of the eyelids typifies Ocular loiasis. [1,2,3,4,6] Other reported ophthalmic manifestations are anterior chamber and presumed orbital involvement, respectively. [7-14] We report a case of a 23-year-old Nigerian female, semi-urban dweller, recently diagnosed of ocular loiasis.
References
Zoure´ HGM, Wanji S, Noma M, Amazigo UV, Diggle PJ, Tekle AH, et al. The Geographic Distribution of Loa loa in Africa: Results of Large-Scale
Implementation of the Rapid Assessment Procedure for Loiasis (RAPLOA). PLoS Negl Trop Dis 2011; 5(6): e1210.
Amazigo U. The African Programme for Onchocerciasis Control (APOC). Ann Trop Med Parasitol. 2008; 102, 1:19–22.
World Health Organization: Onchoc erciasis and its control. WHO Tech RepSer 1995, 852:1-103.
Okonkwo ON, Hassan AO, Alarape T, Akanbi T, Oderinlo O, Akinye A, et al. Removal of adult subconjunctival Loa loa amongst urban dwellers in Nigeria. PLoS Negl Trop Dis 2018; 12(11): e0006920
Samuel Wanji, Nicholas Tendongfor, Theolbald Nji, Mathias Esum, Julious N Che, Armand Nkwescheu, et al. Community-directed delivery of
doxycycline for the treatment of onchocerciasis in areas of co-endemicity with loiasis in Cameroon. Parasites & Vectors 2009, 2:39 doi:10.1186/1756-3305-2-39
Klion AD, Massougbodji A, Sadeler BC, Ottesen EA, Nutman TB. Loiasis in endemic and nonendemic populations: immunologically mediated differences in clinical presentation. J Infect Dis 1991; 163:1318-25.
Omolase CO, Sotiloye OA, Ogunleye OT, Omolase BO. Ocular loiasis in a Nigerian male adult. The N Iraqi J med 2012; 8: 86–90.
Osuntokun O, Olurin O. Filarial worm (Loa loa) in the anterior chamber. Report of two cases. Br j ophthalmol 1975; 59: 166–167.
Pedro-Egbe CN, Chukwuka IO, Obunge OK. Live adult Loa loa in the anterior chamber of a Nigeria female. Port Harcourt medical journal 2008; 3(1): 104–107.
Hassan S, Isyaku M, Yayo A, Sarkin Fada F, Ihesiulor GU, Iliyasu G. Adult Loa loa Filarial Worm in the Anterior Chamber of the Eye: A First Report from Savanna Belt of Northern Nigeria. PLoSNegl Trop Dis 2016; 10(4): e0004436.doi:10.1371/journal. pntd. 0004436
Carme B, Kaya-Gandziami G, Pintart D. Localization of the filaria Loa loa in the anterior chamber of the eye. Apropos of a case. Acta Trop. 1984 Sep; 41(3):265–269.
Barua P, Barua N, Hazarika NK, Das S. Loa loa in the anterior chamber of the eye: a case report. Indian J Med Microbiol. 2005 Jan; 23(1):59–60.
Sandford-Smith J. Eye Diseases in hot climates. 3rd Edition. Oxford: Butterworth-Heinemann; 1997 :270-272.
Otulana TO, Ajibode HA, Bodunde OT, Onabolu OO. Orbital Loiasis masquerading as orbital cellulitis: A Case Series. Annals of Health Research 2016; 2(1): 52-55.
Additional Files
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2024 Transactions of the Ophthalmological Society of Nigeria

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.