A case of central retinal vein occlusion associated with retrobulbar optic neuritis
Abstract
BACKGROUND
Central retinal vein occlusion (CRVO) secondary to retrobulbar optic neuritis is a rare manifestation, and we did not find a reported case from Nigeria in the literature. There are very few reported cases of both pathologies co-existing in the same patient.1-3
CLINICAL PRESENTATION
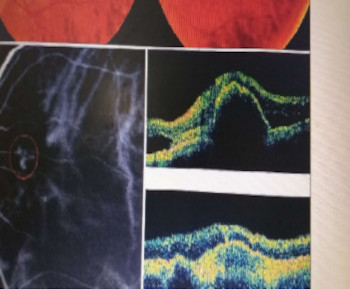
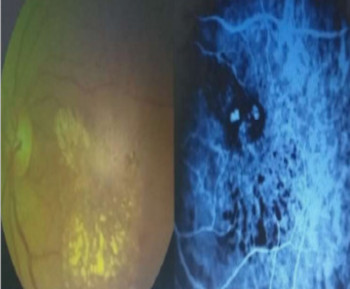
A 58-year-old gentleman, a known glaucoma patient, presented in our clinic with a one-hour history of painless, sudden loss of vision in the left eye. One month prior to the loss of vision, his eye felt heavy, but there was no redness, no pain on ocular movement or reduction in vision. On presentation to the clinic, we examined a middle-aged, healthy-looking man; he had a blood pressure of 130/70 mmHg, and all other aspects of his systemic examination, including the neurological examination, were normal, apart from the ocular examination. Visual acuity was 6/6 in the right eye and counting fingers at 3m (3MCF) in the left eye; intraocular pressures were 20 and 22 mmHg, respectively. His right ocular examination findings were normal. On the left, there was a relative afferent pupillary defect (RAPD), and posterior segment examination revealed a pale disc and cup disc ratio of 0.75, with distinct margins but dilated tortuous venules in all quadrants with mild retinal haemorrhages (Figure 1). Color desaturation was 100:30 and light appreciation was 100:20 in the right and left eyes, respectively. Fundus fluorescein angiography showed a delay in venule filling in all quadrants, worse inferotemporally. There was no area of capillary dropout and no feature suggestive of macula oedema (Figure 2); however, the late images showed hyperfluorescence (Figure 3) in the disc, suggesting an inflammatory process, i.e. retrobulbar neuritis, in the left eye. The optical coherence tomography showed no significant macula oedema (Figure 4). Brain magnetic resonance imaging (MRI) showed nonspecific white matter changes; the MRI spine did not show any significant white matter changes. A diagnosis of left mild central retinal vein occlusion associated with retrobulbar neuritis secondary to multiple sclerosis (Clinical Isolated Syndrome) was made. He was placed on intravenous methylprednisolone 1g daily for 3 days and continued on 60 mg prednisolone daily, which was subsequently tapered off. His vision on the first day after commencing steroids improved to 6/12, and at 2 weeks, his vision had improved to 6/6, although he still had significant visual field changes (Figures 5 and 6). Over the last 4 months of follow-up, the left visual acuity remained 6/6, but he still had significant visual field changes (Figure 7). The patient consented to this case report, and ethical approval was obtained from the research ethics committee of Asokoro District Hospital, Abuja.
DISCUSSION
Although he had features suggestive of a central retinal vein occlusion (CRVO), these could not explain the visual acuity of 3MCF and relative afferent pupillary defect, as the features of CRVO were mild. Retrobulbar neuritis was the main cause of reduced vision because of the visual acuity, RAPD, markedly reduced light appreciation and color desaturation, leakages around the optic nerve head seen in the late stages of FFA and the great improvement on commencing intravenous methylprednisolone.
CONCLUSION
A high index of suspicion is required to rule out retrobulbar neuritis when it co-exists with a retinal vein occlusion that cannot account for the clinical features seen.
References
Duker, J.S., Sergott, R.C., Savino, P.J., & Bosley, T.M. (1989). Optic neuritis with secondary retinal venous stasis. Ophthalmology, 96 4, 475-80.
Rana, V.M., Kim, E.J., Rana, S., Janigian, R.H., Bakaeva, T., & Saade, C. (2023). Pediatric Central Retinal Vein Occlusion Secondary to Concurrent Mechanisms of Optic Neuritis and Antiphospholipid Syndrome. Journal of VitreoRetinal Diseases, 7, 245 - 248.
Lukewich MK, Micieli JA. Venous stasis retinopathy secondary to myelin oligodendrocyte glycoprotein antibody-positive optic neuritis. Retin Cases Brief Rep. 2022;16(3):305-307. doi:10.1097/ICB.0000000000000977
Additional Files
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2025 Transactions of the Ophthalmological Society of Nigeria

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.