Masquerading Orbital Abscess: A Case Report
Abstract
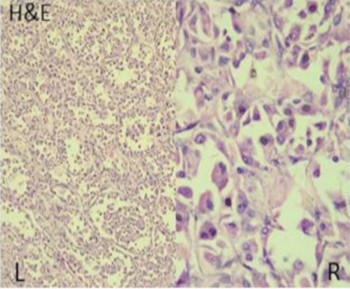
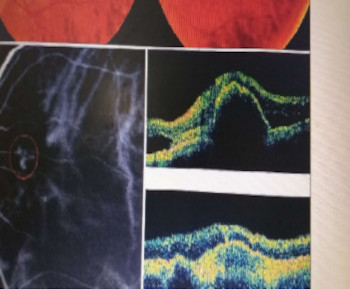
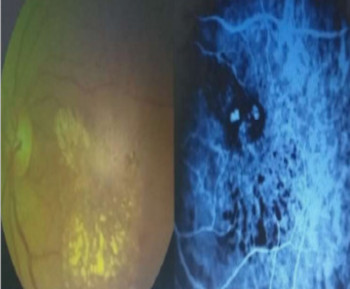
Any purulent collection in the orbit is known as an orbital abscess.1-2 It typically follows an infection of the orbital soft tissues (orbital cellulitis). Classic clinical findings include fever, erythema, proptosis, chemosis, ptosis, restriction of and pain with ocular movement, reduced visual acuity and an afferent pupillary defect.1-4 Orbital cellulitis/abscess is the most common cause of acute-onset proptosis in children.3,4 The differential diagnoses of orbital cellulitis include orbital trauma, for which there may not be a reliable history in children; nonspecific orbital inflammation; benign orbital tumors such as lymphatic malformation and hemangioma; as well as malignant tumors such as rhabdomyosarcoma, leukemia, and metastases.1 Rhabdomyosarcoma is the most common primary orbital malignancy in children.1,5,7,8 This makes it a particularly important differential of orbital cellulitis in addition to its classic presenting picture of sudden onset, rapidly progressive unilateral proptosis. It is associated with marked ocular adnexal inflammatory response in 60% of cases, thereby closely imitating orbital cellulitis.5-7 Herein, we report a case of orbital cellulitis with abscess that mimicked rhabdomyosarcoma in an eleven-year old boy with rapid-onset unilateral proptosis.
References
Foster JA, Carter KD, Durairaj VD, et al. Section 07: orbit, eyelids and lacrimal system. In: Cantor LB, Rapuano CJ, Cioffi GA, editors. 2016–2017
Basic and Clinical Science Course. San fransisco: American Academy of Opthalmology; 2016:70– 72.
Hegde R, Sundar G. Orbital cellulitis- A review. TNOA J Ophthalmic Sci Res 2017; 255:211-219.
Nageswaran S, Woods CR, Benjamin DK Jr., Givner LB, Shetty AK. Orbital cellulitis in children. Pediatr Infect Dis J. 2006; 25(8):695–699. doi:10.1097/01.inf.0000227820.36036.f1
Jain A, Rubin PA. Orbital cellulitis in children. Int J Ophthalmol Clin. 2001; 41(4):71–86. doi:10.1097/00004397-200110000-00009
Bajaj MS, Pushker N, Chaturvedi A, et al. Orbital space occupying lesion in Indian children. J PediatrOphthalmol Strabismus. 2007; 44:106–
Boparai MS and Dash RG. Clinical, ultrasonographic and CT evaluation of orbital rhabdomyosarcoma with management. Indian J Ophthalmol. 1991; 39:129–131.
Lueder GT, Archer SM, Hered RW, et al. Section 06: pediatric ophthalmology and strabismus. In: 57 Cantor LB, Rapuano CJ, Cioffi GA, editors. 2016– 2017 Basic and Clinical Science Course. San fransisco: American Academy of Ophthalmology; 2016: 313–314.
Amir SP, Kamaruddin MI, Akib MNR, Sirajuddin J. Orbital cellulitis clinically mimicking Rhabdomyosarcoma. International Medical
Case Reports Journal 2019; 12: 285–289
Wikipedia contributors. Pus. Wikipedia, The Free Encyclopedia. November 5, 2019, 04:32 UTC. Available at: https://en.wikipedia.org/w/
index.php?title=Pus&oldid=924659971. Accessed November 15, 2019.
Khan AA, Alsahli MA, Rahmani AH. Myeloperoxidase as an Active Disease Biomarker: Recent Biochemical and Pathological
Perspectives. Med Sci (Basel). 2018; 6(2):33. doi:10.3390/medsci6020033