Paediatric corneal transplantation in Uyo, Nigeria: A report of two cases
Abstract
Introduction: Corneal blindness is one of the top 5 causes of blindness globally1,2. It is the fourth leading cause of blindness in Sub-Saharan Africa (SSA)2, and third leading cause of blindness in Nigeria3. Children are not spared4-6. Unfortunately, corneal banking services are still quite rudimentary in SSA including Nigeria7,8. Corneal transplant, particularly penetrating keratoplasty (PKP), has been found to be a very
useful vision restoration surgical procedure in cases of corneal opacity, even in children 8-12. However, in children vision restoration is often
further facilitated by appropriately managing co- morbidities related to blinding corneal disease in childhood9,10. PKP in children has been largely noted to be uniquely challenging. These challenges include: the need for multiple examinations under general anaesthesia (GA) to review the surgical site, recipient and graft tissue, remove corneal sutures and frequent requirement of combined management of stimulus deprivation amblyopia. Others are increased risk of failure from graft dehiscence, graft infection, graft rejection, technical complexity of the procedure due to scleral elasticity, as well as the dependence on caregivers’ commitment to immediate post- operative care and long-term follow-up9-13. Despite these challenges successful outcomes of PKP in children have been reported 9-12 . Only few successful cases of PKP in children have been reported in Nigeria. Hence this report of our initial experiences with penetrating keratoplasty in 2 children with blinding corneal diseases in Uyo, Nigeria.
Case report: This is a descriptive report of 2 Nigerian children with blinding corneal diseases who had undergone PKP for visual restoration at Zerah International Eye Hospital (ZIEH), Uyo, Akwa Ibom State, Nigeria in March, 2019. The first case was a 10-year-old out-of-school male
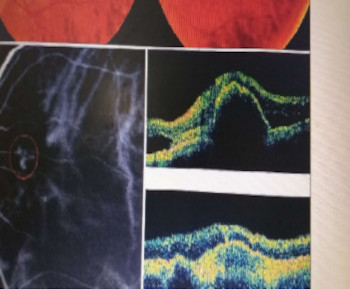
who presented with history of bluish coloured, ‘cloudy eyes’ from birth, poor vision and roving eye balls. Significant ophthalmic findings included pendular nystagmus, visual acuities (VA) of 1/60, N48 OD and 3/60, N48 OS. Both corneae had a uniform ground glass appearance and diffuse corneal stromal oedema (denser in the right eye). The pachymetry readings averaged 1067nm OD Figure 1a, b and c: Bilateral congenital hereditary endothelial dystrophy in a 10-year-old male pre-operative (right and left eye) and right post-operative PKP.
and 1075nm OS. A diagnosis of bilateral congenital hereditary endothelial dystrophy (CHED) was made. He had right PKP under GA (Figure 1). The BCVA of his right eye improved from 1/60 at presentation to 6/60 at 3 months post-operative and has remained 6/24 from 6 months post- operative until his 3-year post-operative visit. His near VA improved from N48 to N10 with the best refractive correction using spectacles. He has since started elementary school. As at the time of writing this report, the plans for performing left PKP procedure (although delayed due to multiple contributory financial and social constraints) were underway. The second case was a 3-year-old male who
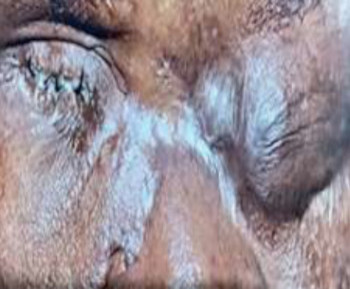
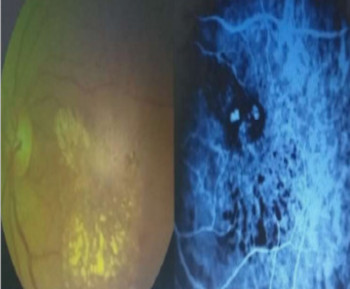
presented with a profound poor vision in the left eye following left herpes simplex keratitis 1 year prior to presentation. Examination revealed VA of light perception (LP)-OS, 35-40 prism diopters left sensory, concomitant esotropia, and left central leucoma 4-5mm in diameter. He had left PKP under GA (Figure 2). He made remarkable improvement with BCVA improving from LP to 6/60, 6/18 and
6/12 at 6 months, 1 year and 3 years post- operatively, after refractive correction and amblyopia therapy with patching.
Conclusion: Albeit the challenges, successful paediatric corneal transplantation can be performed in resource-limited settings. Paediatric
corneal transplantation can significantly improve vision as is reported in our cases.
References
World Health Organization. (2019). World report on vision. World Health Organization. Available at https://apps. who.int/ iris/han dle/1066 5/328717. [cited 2023 June 20]
Flaxman SR, Bourne RRA, Resnikoff S, Ackland P, Braithwaite T, Cicinelli MV, et al. Global causes of blindness and distance vision impairment 1990-2020: a systematic review and meta-analysis. Lancet Glob Health. 2017; 5(12):e1221- e1234.
Abdull MM, Sivasubramaniam S, Murthy GV,Gilbert C, Abubakar T, Ezelum C, Rabiu M. Causes of Blindness and Visual Impairment in Nigeria: The Nigeria National Blindness and Visual Impairment Survey. Invest Ophthalmol Vis Sci. 2009; 50:4114–4120
Onabolu ROO, Iwuora NA, Ceesay W. Corneal Diseases in Children in The Gambia. Niger J Ophthalmol.2009; 17(1): 1-4
Bella AL, Dohvoma VA, Eballe AO, Abdouramani O. Pattern of corneal pathologies in children seen at Yaoundé Gynaeco-Obstetric and Paediatric Hospital, Cameroon. Clinical Ophthalmology 2013; 7: 2007–2010 92
Shah A, Chaudhary M, Shreshtha JK. Pattern of Corneal Diseases in Paediatric Age Group at a Tertiary Eye Care Center in Nepal. Nepal J Ophthalmol 2017; 9(17): 37-42
Waziri-Erameh JM, Omoti AE, Chukwuka IO. The problem of retro- prosthetic membrane following keratoprosthesis in Nigerian eyes.
American Journal of Case reports. 2008; 9:211-215.
Umana UI, Ezeh EI, Nkanga DG, Utam UA, Ibanga AA, Etim BA, et al. Early experience with penetrating kerato- plasty in South-South Nigeria: Initial audit of indications and outcome. Arch Int Surg 2018; 8:101-107.
Mun-Wei L, Md Said H, Punitan R, Ibrahim M, Shatriah I. Indications, Clinical Outcomes, and Survival Rate of Pediatric Penetrating Keratoplasty in Suburban Malaysia: A 10-year Experience. Cureus 2018; 10(12): e3744. DOI 10.7759/cureus.3744.
Trief D, Marquezan MC, Rapuano CJ, Prescott CR. Pediatric corneal transplants. Current Opinion in Ophthalmology 2017; 28(5):477-484.
doi: 10.1097/ICU.0000000000000393.
Sharma A, Sharma R. pediatric corneal transplant surgery: Challenges for successful outcome. Nepal j Ophthalmol 2019; 11(22):197-210.
Al-Ghamdi A, Al-Rajhi A, Wagoner MD. Primary pediatric keratoplasty:indications, graft survival, and visual outcome. J AAPOS. 2007; 11(1):41-7. doi: 10.1016/j.jaapos.2006.09.012. PMID: 17307682.
Zhu AY, Marquezan MC, Kraus CL, Prescott CR. Pediatric Corneal Transplants: Review of Current Practice Patterns. Cornea. 2018; 37(8): 973-980.
Downloads
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2023 Transactions of the Ophthalmological Society of Nigeria

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.