Comparison of Arclight Loupe vs Traditional Direct Ophthalmoscope in evaluation of Corneal Epithelial Defects by General Practitioners: a proposal synopsis
Abstract
BACKGROUND
Corneal blindness is the 5th, 4th and 3rd leading cause of blindness globally, in Sub-Saharan Africa and Nigeria, respectively.1-3 Globally, corneal epithelial defects (CEDs), particularly corneal ulcers, constitute the major cause of corneal blindness.4 Regrettably, under-resourced areas and low- and middle-income countries (LMICs) with the least capacity to manage corneal lesions bear the greatest burden.4 Therefore, in order to encourage timely diagnosis of CEDs, the use of the +10 dioptre lens of the traditional direct ophthalmoscope (TDO) along with fluorescein dye has been advocated for use by non-ophthalmologists in the evaluation of suspected corneal lesions.5
Unfortunately, TDO use by non-ophthalmologists, including the general practitioners (GPs), the first-line physicians, is grossly limited. TDO skills deficiency, its bulk, relatively high cost, and sophistication are largely implicated.6 Arclight Loupe (AL), a portable, relatively low-cost and less sophisticated multipurpose diagnostic tool consisting of an anterior segment loupe, ophthalmoscope and otoscope, offers a reliable alternative to TDO.7 However, its utility in CEDs by GPs has not been assessed.
OBJECTIVE
To compare the utility of AL vs TDO in the clinical examination of corneal epithelial defects by GPs.
METHODS
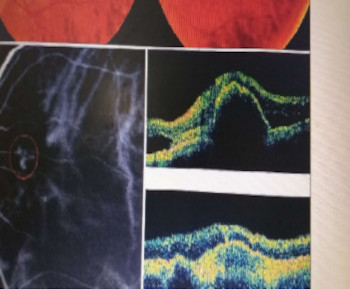
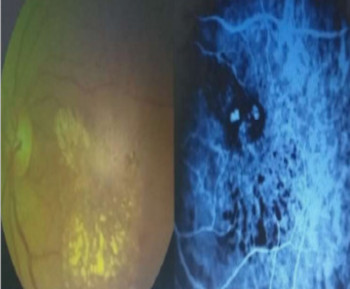
A comparative cross-sectional study shall be undertaken. The study shall adhere to the tenets of the Declaration of Helsinki, and ethical approval shall be obtained from the Institutional Review Board of the University of Calabar Teaching Hospital, Calabar. Ten (10) TDO-exposed GPs will be recruited, trained and subsequently randomly assigned into two groups of 5 GPs each (group 1 & group 2). A cross-over design will be utilised in which group 1 uses the Arclight (Figures 1 and 2) first and subsequently the TDO, while group 2 will use the instruments in the reverse order.
Study subjects (CED+ve vs CED-ve) shall be consecutively recruited and independently examined by the GPs. Three experienced Ophthalmologists (SL1-3) shall work together examining each consecutive subject with the Slit Lamp to establish the CED parameters (presence/location/shape/size/depth) as the “reference standard”.
This study will compare the Arclight loupe to the Welch Allyn 11720-VC ophthalmoscope in terms of four measures: (1) accuracy of CED parameters (compared against the “reference standard”), (2) ease of examination (EOE) for the examiners (GPs) using a score of 1–8, (3) ease of use (EOU) for the examiners (GPs) using a score of 1–5, (4) ocular comfort level (OCL) as determine by the level of glare experienced by the subject using a score of 1–4, and (5) length of examination (LOE) as determined by the subject’s perceived duration of the assessment using a score of 1–4.
RESULTS
Data obtained shall be entered and appropriately analysed with STATA/IC version 15.0.
CONCLUSION
The prospective utility in the diagnosis of corneal epithelial defects using AL compared to TDO among GPs in our environment shall be objectively ascertained.
References
World Health Organization. (2019). World report on vision. World Health Organization. Available at https://apps.who.int/iris/handle/10665/328717. [cited 2024 August 20]
Flaxman SR, Bourne RRA, Resnikoff S, Ackland P, Braithwaite T, Cicinelli MV, et al. Global causes of blindness and distance vision impairment 1990-2020: a systematic review and meta-analysis. Lancet Glob Health. 2017; 5(12): e1221-e1234.
Abdull MM, Sivasubramaniam S, Murthy GV, Gilbert C, Abubakar T, Ezelum C, Rabiu M. Causes of Blindness and Visual Impairment in Nigeria: The Nigeria National Blindness and Visual Impairment Survey. Invest Ophthalmol Vis Sci. 2009; 50:4114–4120.
Wang EY, Kong X, Wolle M, Gasquet N, Ssekasanvu J, Mariotti SP, Bourne R, Taylor H, Resnikoff S, West S. Global Trends in Blindness and Vision Impairment Resulting from Corneal Opacity 1984-2020: A Meta-analysis. Ophthalmology. 2023; S0161-6420(23): 00187-2.
Timlin H, Butler L and Wright M. The accuracy of the Edinburgh red eye diagnostic algorithm. Eye 2015; 29(5): 619–624.
Alizadeh Y, Akbari M, Dourandeesh M, Aleali M. Do General Practitioners have Sufficient Knowledge and Skills in Using Direct Ophthalmoscope? A Survey on General Practitioners of Northern Iran. Int J Med Invest 2021; 10 (2): 156-165
Lowe J, Cleland CR, Mgaya E, Furahini G, Gilbert CE, Burton MJ, et al. The Arclight Ophthalmoscope: A Reliable Low-Cost Alternative to the Standard Direct Ophthalmoscope. J Ophthalmol. 2015. https://doi.org/10.1155/2015/743263
Additional Files
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2025 Transactions of the Ophthalmological Society of Nigeria

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.